When there is suspicion of PCOS and a pelvic ultrasound is required to assess the ovarian appearance, it is valuable to understand how to identify specific ultrasound characteristics associated with PCOS. The presence of just one polycystic ovary can raise concerns.
When performing a transvaginal ultrasound for suspected PCOS (polycystic ovary syndrome), the objective is to assess the presence of an excessive quantity of small follicles on the ovaries, a characteristic feature of this condition. This diagnostic imaging procedure entails the insertion of a probe into the vagina to obtain an internal view of the ovaries.
It’s important to note that ultrasound findings alone are insufficient to definitively confirm the presence of PCOS. These results constitute a significant piece of the diagnostic puzzle, alongside other essential factors such as your medical history, a physical examination, and the findings from blood tests, all of which your healthcare provider will consider in reaching a diagnosis.
Understanding Polycystic Ovary Syndrome
Polycystic ovary syndrome (PCOS), also referred to as polycystic ovarian syndrome, is a prevalent health condition stemming from an imbalance in reproductive hormones. This hormonal disruption adversely affects the functioning of the ovaries, which are responsible for producing the egg released during a typical menstrual cycle. In individuals with PCOS, the egg may not mature correctly, or it may fail to be released during ovulation as expected.
These irregularities in menstrual cycles can lead to:
- Infertility, as PCOS ranks among the most common causes of infertility in women.
- Formation of cysts which are nothing but your immature follicles. Which dissolve on their own. Sometimes they may turn into a large fluid-filled simple cyst which mostly resolves on its own or needs medication.
The Role of an Ultrasound in Diagnosing PCOS
When performing imaging to evaluate polycystic ovaries, transvaginal ultrasound is considered the preferred method, known as the gold standard, due to its superior ability to visualize the internal structure of the ovaries, especially in patients who are obese. In comparison to transabdominal ultrasound, transvaginal ultrasound is more effective at identifying the characteristic appearance of polycystic ovaries in women with PCOS.
In cases where transabdominal ultrasound is necessary, typically due to a patient’s lack of sexual activity or personal preference against transvaginal examination, it is crucial to ensure that the bladder is appropriately filled but not overly distended. Overfilling the bladder can exert pressure on the ovary, potentially causing deviations from the typical ellipsoid model used for calculating ovarian volume.
The incorporation of 3D ultrasound into the transvaginal examination further simplifies the assessment and imaging necessary for precise PCOS diagnosis. This advanced technology allows for the precise counting of individual follicles and accurate calculation of ovarian volumes through software, significantly reducing the likelihood of errors in PCOS ultrasound images.
Characteristics of PCOS on Ultrasound
A polycystic ovary typically exhibits one or more of the following ultrasound features:
- The presence of 12 or more ovarian follicles (measuring 2—9 mm) arranged peripherally within the ovary, resembling a string of pearls.
- An increased ovarian volume exceeding 10 cm^3.
- A hyperechoic stroma.
The most conspicuous ultrasound sign is often the first one, where ovarian follicles appear more prominent than normal and are aligned along the periphery of the ovarian tissue. In some cases, these follicles can multiply to the extent that they resemble a cluster of grapes (which is another term used to describe the appearance of PCOS on ultrasound), further contributing to the enlargement of the ovary beyond 10 cm^3.
Different Diagnoses and Limitations
Internal Transvaginal Ultrasound
An internal transvaginal ultrasound offers doctors a much closer examination of your uterus and ovaries, and it is the most common method for diagnosing PCOS. The term ‘transvaginal’ essentially means ‘through the vagina’. During this procedure, you lie on your back with your knees raised, and a small ultrasound probe is gently inserted into the vagina. While these procedures may seem intimidating and can cause mild discomfort, it is advisable to try and stay relaxed. Typically, the procedure is painless and brief. However, if you experience discomfort upon insertion or at any point during the scan, it’s important to promptly inform the health care provider. They then would be conducting the examination.
Doctors prefer this method over external ultrasound for diagnosing PCOS due to the unique characteristics of the condition. The cysts associated with PCOS are typically situated just beneath the surface of the ovaries and are generally no larger than 8 mm in diameter. These cysts are essentially follicles containing eggs that have not developed properly due to hormonal imbalances and fail to release during ovulation. Instead, they remain in an immature state, resembling small cysts arranged in a radial pattern just beneath the surface, encircling the ovary’s edge. Because of the small size and location of these cysts, a transvaginal ultrasound offers a clearer indication of PCOS to your doctor compared to an external ultrasound.
External Ultrasound
An external ultrasound scan is the more familiar type of ultrasound for most people. It is commonly used for monitoring the health of an unborn baby during pregnancy and can also be employed to examine other internal organs for diagnosing potential ailments, such as appendicitis. In this scan, a gel is applied to your skin, and a handheld probe is moved across the area of your body being examined. The gel aids in facilitating the transmission of high-frequency ultrasound waves, resulting in clearer images.
The Differences
While the transvaginal ultrasound procedure is more invasive than an external ultrasound, it offers the best opportunity for an accurate diagnosis. A transvaginal ultrasound provides your doctor with a more comprehensive understanding of your reproductive health, which in turn can enhance the management of your condition.
Other Possible Findings
A transvaginal ultrasound is employed to assess internal structures when screening for PCOS. During the procedure, the sonographer will evaluate your uterus, cervix, and ovaries. They will also determine the number of follicles on your ovaries, which is referred to as the antral follicle count (AFC).
Antral follicles are dormant follicles present in the ovary at the start of every menstrual cycle. They typically measure around 2 to 9 millimeters in size, which is slightly less than half an inch.
Next Steps After Your Appointment
Diagnostic Procedures
Before confirming a PCOS diagnosis, your healthcare provider may request a variety of tests tailored to your specific symptoms and medical history.
Blood Tests
Blood tests can help identify elevated androgen levels through measurements of testosterone and the free androgen index (FAI). Additionally, blood tests may assess other reproductive hormones that impact your menstrual cycle, such as estrogen (the female sex hormone) and follicle-stimulating hormone (FSH). These tests are essential for understanding hormonal imbalances.
Your healthcare provider might also recommend blood tests to rule out conditions that share symptoms with PCOS. It’s worth noting that if you are currently taking oral contraceptives, you’ll need to discontinue them for three months before undergoing hormonal blood tests.
Ultrasound
To detect signs of PCOS, your doctor or specialist may perform an abdominal ultrasound. This imaging technique can reveal indicators like partially developed eggs on your ovaries, enlarged ovaries, or a thickened uterine lining. In cases where the patient is sexually active, a transvaginal ultrasound may be utilized.
Additional Assessments
Your healthcare provider may conduct assessments to evaluate your risk of developing cardiovascular disease and type 2 diabetes. These assessments may include:
- Cholesterol Blood Test
- Blood Pressure Measurement
- Glucose Tolerance Test
If you are diagnosed with PCOS, it is advisable to undergo cholesterol and diabetes tests every few years, along with an annual blood pressure check. If you have specific risk factors, such as a family history of diabetes or previous abnormal cholesterol results, or if you are planning a pregnancy, your healthcare provider may recommend more frequent testing.
Consult a PCOS Doctor
PCOS can be diagnosed by medical specialists such as gynecologists, endocrinologists, or reproductive endocrinologists, all of whom have received specialized training in assessing and managing hormonal disorders.
If you have doubts or concerns about your PCOS diagnosis, or if you have not received a definitive diagnosis, seeking a second opinion can be a prudent course of action. Doctors at Veera Health advocate for transparent and open communication. This enables patients to feel empowered in making well-informed decisions regarding their health. They are committed to offering support by lending an empathetic ear and engaging in collaborative decision-making with patients throughout their healthcare journey. They hold a strong passion for holistic well-being and the potential for natural remedies. Such simple lifestyle adjustments often yield significant improvements in overall health outcomes and enhance one’s quality of life.
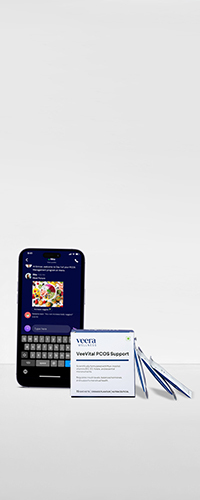
Learn More With Veera
The medical professionals at Veera Health are continually exploring options to facilitate your journey toward reversing PCOS, whether through medication or natural approaches.
Disclaimer: Please be aware that the content on Veera is presented for informational purposes exclusively and should not be construed as medical guidance or a replacement for advice from a qualified physician.