Don’t want to get pregnant any time soon? You can opt for an implant which is the most effective method of birth control (other than abstinence) at preventing unwanted pregnancy – 99.9% effective! It can be an excellent alternative for birth control pills and a superb option for breastfeeding mums. Here’s all you need to know about this form of contraception.
What is an implant and how does it work?
Implanon vs. Nexplanon
An implant is a hormonal contraceptive with brand names like Implanon and Nexplanon. Doctors insert a matchstick-like, piece of plastic under the skin, usually in the upper arm. Once the implant is inserted, it releases a steady stream of hormones that prevent the ovaries from releasing eggs and thickens cervical mucus, thus preventing unwanted pregnancies. Once the hormones enter your system, they stay steady until you remove the implant.


When should an implant be inserted?
Doctors will first ensure that you are not pregnant before inserting the implant into your arm. Before doctors start the procedure, they inject a little local anesthetic in your arm so that you do not feel any pain during the insertion. It will feel like getting a vaccine and your arm will feel sore for a day or so after the insertion. You can get it at any point in your menstrual cycle, but depending on where you are in your cycle, you may need an additional non-hormonal contraceptive method like a condom for the following seven days. Consult with a doctor to ensure you’re clear on how long you will need an additional contraceptive.
What are the benefits of getting an implant?
An implant can last for about 3-5 years so that you can forget about worrying about contraception in your foreseeable future. An implant can be a great choice if you tend to forget to take the pill every day or if you don’t want to interrupt foreplay with a condom. And although you will be able to feel the implant bar under your skin, you will not be able to see it, nor will other people notice!
Are there any side effects of this form of birth control method?
- Just like the IUD or contraceptive pill, the implant does not protect against sexually transmitted infections (STIs), therefore be sure to use a condom if you don’t know your partner’s status
- The most common complaint women have is irregular bleeding – some women have light spotting, lighter periods or no periods, but some may have heavier, crampier periods.
- Like other hormonal contraceptives, you may suffer from acne, mood swings, weight gain and changes in sexual desire. These however tend to improve after the first few months of use.
- You may be a little bruised during the time of insertion or removal but it will resolve in a few weeks. Sometimes, after the removal you can get a small scar.
How soon after removing the implant can you get pregnant?
Once you remove the implant, the contraceptive effect wears off quickly. Your fertility returns to normal within one cycle, and you can get pregnant. Make sure to use an additional form of contraception, like a condom, once you take the implant out if you do not intend to get pregnant.
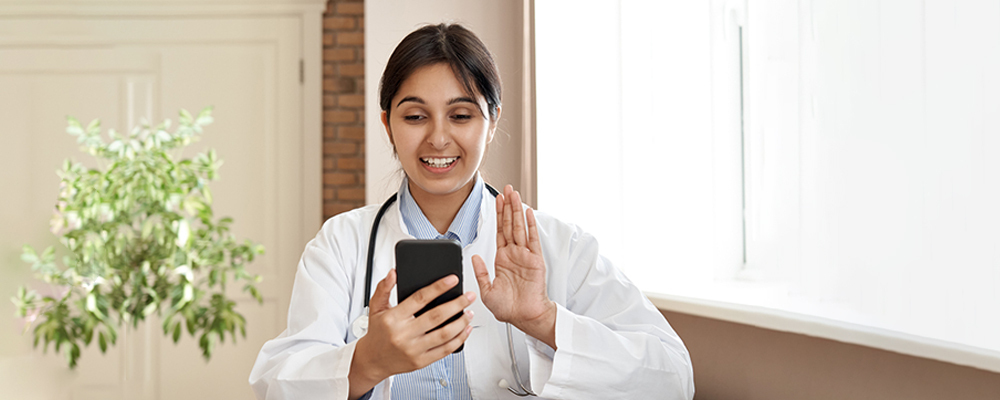
Learn More with Veera Health
Finding the right type of contraception may need several trials using different methods to land on what works best for you. You can book an appointment with one of the doctors on our portal to talk about what’s important to you when it comes to birth control.
Reviewed by: Dr. Shailly Prasad, MD/MBA, Resident Physician, Obstetrics & Gynecology.
Disclaimer: Content on Veera is provided for informational purposes only and is not intended as medical advice or as a substitute for medical advice given by a physician or trained professional.
References:[1] Hohmann H, Creinin MD. The contraceptive implant. Clin Obstet Gynecol. 2007 Dec;50(4):907-17. Review. PubMed PMID: 17982333.[2]Hohmann H. (2009). Examining the efficacy, safety, and patient acceptability of the etonogestrel implantable contraceptive. Patient preference and adherence, 3, 205–211. https://doi.org/10.2147/ppa.s4299[3] Practice Bulletin No. 186: Long-Acting Reversible Contraception: Implants and Intrauterine Devices. (2017). Obstetrics & Gynecology, 130(5). doi:10.1097/00006250-201711000-00053