Losing weight with Polycystic Ovarian Syndrome (PCOS) can seem like an uphill battle. Despite trying every diet available online, going gluten & dairy-free, exercising every day of the week, the weight keeps piling on. If you’re wondering what’s going on, you’re not alone. Unfortunately, regular weight loss diets don’t always work for women with PCOS. This is because your hormones are working against you and PCOS is a complex condition. It’s hard to create and follow a diet for PCOS that can help balance these hormones all by yourself.
If you’ve done some reading on PCOS, then you’ve likely come across the term ‘insulin resistance’. In particular, if you have weight struggles or persistent belly fat, it’s time you get to know this health condition better. That’s because insulin resistance is common in women with PCOS, and the two often go together. First, let’s start with the basics.
The PCOS and insulin relationship
PCOS is an endocrine disorder related to hormones. Hormones are small molecules that the body makes and releases into your bloodstream to communicate to another organ to do some sort of function. With PCOS, the hormones that regulate your period go out of whack, causing irregular periods and a rise in male hormones like testosterone (androgens). This further causes excessive facial hair, acne and increased insulin, a vital hormone with many different functions.
Now, let’s talk about insulin. Insulin regulates how the body processes food. When you eat something, glucose or sugar is released into your bloodstream after digestion. But it’s not enough for glucose to be in your blood; to get energy from food, your cells need to also absorb the glucose from the blood. This is where insulin comes in. Insulin is released by the pancreas to help the cells in your body absorb this glucose from the blood stream and get energy from it.
What Is Insulin Resistance?
Insulin resistance means that your body’s cells do not respond as well, or at all, to insulin anymore. As a result, the glucose stays in the bloodstream, without being absorbed by cells. This means that even though you’ve eaten, your body feels tired and your brain craves more food because glucose isn’t getting converted to energy. Eventually this high level of glucose in the blood can cause diabetes. Untreated diabetes, the end result of insulin resistance, can cause damage to the eyes, nerves, kidneys, and increase your risk of infections and heart disease.
Understanding Obesity and Hormonal Belly Fat
Insulin is also a hormone that affects your appetite and so if you no longer respond to insulin, so your body compensates by making more of it. When you have too much insulin in your body (aka hyperinsulinemia), you feel hungry and crave sweet things to increase your blood sugar (even though your blood sugar is already high and your body is just not absorbing it).
It’s important to realize that obesity is linked to insulin resistance because the body has plenty of fat stores and glucose available. At some point, the body cannot keep up with producing and responding to insulin appropriately. Approximately 50% of women with PCOS are obese, and about 70% of women with PCOS have insulin resistance. But you don’t necessarily have to be obese to have insulin resistance!
Another factor affecting weight loss is hyperandrogenism. This condition happens when you have excessive male hormones. As you know, increased testosterone and androgens cause an abnormal rise in facial hair and acne. This surge in male hormones also promotes fat storage in the abdomen area. So, if you’ve been regularly exercising and still fighting a stubborn muffin top, insulin resistance is most likely the cause.
So what should I do?
You’ve probably heard this before but the best way to lose weight and manage PCOS long-term is through lifestyle changes like regular exercise, healthy eating, managing stress levels and getting adequate sleep. For women without lean PCOS, losing just 5-10% of your body weight, even if you’re not obese, can regulate your cycles and decrease your risk of diabetes and heart disease. For women with lean PCOS, exercising and de-stressing can help reduce insulin insensitivity and regulate cycles as well. Gynecologists’ can also prescribe medications such as metformin that help with insulin resistance and weight loss.
Lifestyle & Diet Changes
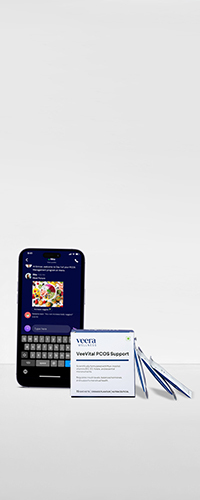
Lifestyle change are harder than they seem, however, and most women struggle to find the right lifestyle habits, and stay consistent. Gluten-free, diary-free diets, seed cycling and other diets are often shared as the holy grail but are NOT required to reverse PCOS. In fact, cutting food groups out of your diet can make food cravings worse. Instead, a diet with low glycaemic index foods that works for YOUR body is better than trying generic ones found online. Working with doctors experienced with PCOS, and a dietician who can give you a personalised PCOS food plan, works wonders in losing weight. Reversing PCOS today is always better than waiting to develop further complications like diabetes, pregnancy complications and potentially cancer.
Learn More with Veera Health
Read our article on options for treatment for PCOS. And if you want to learn more about treatment options, schedule a free consultation with a PCOS expert at Veera Health.