PCOS, exclusive to women, and IBS, affecting twice as many women as men, share intriguing connections. PCOS, marked by irregular menses due to heightened FSH and LH hindering ovulation, may intertwine with IBS, as the same hormones can cause constipation by delaying digestive system movement. Both conditions significantly impact the quality of life, sharing symptoms of bloating, abdominal pain, and bowel habit changes from inflammation. Chronic inflammation in PCOS leads to various health risks, including insulin resistance and heart problems. Moreover, studies link PCOS to intestinal permeability and gut bacteria alterations, a phenomenon also associated with IBS, potentially unleashing toxins into the bloodstream, contributing to symptoms in both conditions.
Understanding the Gut Microbiome
Microorganisms, commonly known as microbes, encompass bacteria, viruses, fungi, and other tiny living entities. Predominantly residing within your intestines and on your skin, trillions of these microbes cluster, with a significant concentration in the cecum, a segment of your large intestine, collectively referred to as the gut microbiome. There are approximately 40 trillion bacterial cells compared to 30 trillion human cells. The human gut microbiome hosts up to 1,000 bacterial species, each playing distinct roles, ranging from vital contributions to potential disease triggers. Collectively weighing as much as 2–5 pounds, equivalent to your brain’s weight, these microbes function as a supplementary organ, wielding significant influence over your health.
What Are Gut Microbiota or Flora?
The gut microbiota exhibits less diversity compared to microbial communities in certain other bodily locations, displaying a notable level of functional redundancy. A comprehensive examination of the functional capacity of the human gut microbiome recently yielded a catalogue of 9,879,896 genes, utilizing data from 249 newly sequenced and 1018 previously published samples. This study identified country-specific microbial signatures, implying that environmental factors, including diet, and potentially host genetics contribute to shaping the composition of the gut microbiota. It’s important to acknowledge that microbiotas with distinct compositions may still share functional redundancy, resulting in comparable protein or metabolite profiles.
Gut microbes play a multifaceted role in human health, influencing various aspects of our well-being. One crucial function lies in nutrition, as these microbes assist in breaking down complex molecules from foods like meats and vegetables, aiding in the absorption of essential nutrients. The diversity of an individual’s diet significantly impacts the diversity of their gut microbiota. Moreover, the gut microbiota plays a pivotal role in the development of immunity. Research suggests that the body’s initial exposure to microbes may commence before birth, contributing to the formation of adaptive immunity that responds effectively to disease-causing organisms. Disruptions to these early microbial exposures can hinder the proper development of the microbiota, potentially affecting immunity.
Beyond physical health, the intricate communication between a person’s gut microbiota and brain through the gut-brain axis extends to behavioural aspects. While the gut-brain axis primarily influences intestinal function, emerging research links the gut microbiota to psychological disorders such as depression and Autism Spectrum Disorder (ASD). Furthermore, the gut microbiota’s impact is evident in disease development, including gastrointestinal conditions like inflammatory bowel diseases (IBD), obesity, and type 2 diabetes.
The status of the gut microbiota is also linked to metabolic syndrome, and dietary modifications involving prebiotics, probiotics, and supplements may mitigate associated risk factors. However, disrupting the microbiota with antibiotics can lead to diseases, including antibiotic-resistant infections. Notably, the microbiota acts as a defence mechanism against the overgrowth of externally introduced populations that could cause disease, as “good” bacteria compete with the “bad,” releasing anti-inflammatory compounds in the process. Understanding and maintaining the delicate balance of the gut microbiota emerge as critical elements for overall health and well-being.
How PCOS Relates To Gut Health
Various factors can influence the composition of microbes residing in our gut, including our dietary choices, sex hormones, sleep quality, geographical location, and body weight. While the gut microbiome was initially perceived primarily as a digestive aid, it is now recognized as a complex contributor to our overall health.
Recent research indicates that women with polycystic ovary syndrome (PCOS) tend to exhibit less healthy dietary patterns compared to those without PCOS, and they are more prone to being overweight or obese.
One recent hypothesis regarding the connection between the gut microbiome and PCOS suggests that an unhealthy diet may disrupt the balance of bacteria in the gut, leading to a condition known as gut dysbiosis. According to this theory, this imbalance could potentially render the gut lining more permeable, allowing harmful substances from specific bacteria to seep into the bloodstream, commonly referred to as a “leaky gut.”
Subsequently, this phenomenon may activate the immune system, interfere with insulin function, resulting in elevated insulin levels, increased production of male hormones in the ovaries, and disruptions in the ovarian process of egg formation.
Common Gut Issues
Irritable bowel syndrome
The primary symptom of Irritable Bowel Syndrome (IBS) is abdominal pain, which can occur before or after bowel movements. Individuals may also experience diarrhoea, constipation, or a combination of both, with the predominance of one determining the type of IBS. Additional symptoms include bloating, the presence of white mucus in the stool, and a sense of incomplete bowel movements. Various factors, including traumatic life events, mental health conditions, infections, or Small Intestinal Bacterial Overgrowth (SIBO), can contribute to the development or exacerbation of IBS symptoms. Given the diverse origins of IBS, different individuals may find relief through personalized approaches, such as making dietary adjustments, learning stress reduction techniques, or addressing underlying conditions to effectively manage their symptoms.
Constipation
Constipation is characterized by infrequent or uncomfortable bowel movements. Typically, an individual is deemed constipated when the passage of small amounts of hard, dry stool occurs, happening less than three times a week. Nevertheless, what constitutes normal stool elimination varies from person to person and can involve having a bowel movement either three times a day or three times a week.
Diarrhea
The human microbiota, primarily composed of bacteria in the gut, consists of 10-100 trillion symbiotic microbial cells. This intricate system continually influences digestion, metabolism, inflammation, and overall systemic responses in the body. An imbalance in the gut microbiome, known as gut dysbiosis, often triggered by bacterial overgrowth, can lead to chronic diarrhoea. This disruption hampers normal digestive tract function as harmful bacteria surpass beneficial ones. Whether resulting from acute or chronic diarrhoea, the loss of gut bacteria exacerbates gut dysbiosis, creating an uncomfortable negative feedback loop. Proactive and reactive probiotic supplementation is crucial, as any form of chronic diarrhoea, regardless of its origin, can have lasting effects on overall health.
Gas & Bloating
Excessive intestinal gas is the primary culprit behind stomach pain and bloating, especially after meals. If you experience a swollen abdomen post-eating, it could indicate a digestive problem. This may stem from factors like overeating rapidly, or it could indicate food intolerance or another condition leading to the accumulation of gas and digestive contents.
Abdominal pain
Alterations in the gut bacteria of individuals experiencing painful gastrointestinal conditions, such as inflammatory bowel disease and irritable bowel disease, have long been acknowledged. However, recent investigations focusing on distinct painful ailments like fibromyalgia, inflammatory pain, headaches, neuropathic pain, and even opioid tolerance have further substantiated the connection between gut bacteria and various forms of chronic pain.
Scientists in this field posit that signaling molecules, derived from microbiota (cells constituting the microbiome), metabolites (directly originating from our diet), neurotransmitters, and neuromodulators, play a role in regulating peripheral and central sensitization. This regulation influences the onset and persistence of pain. These researchers suggest that modifying diet and incorporating specific probiotics may potentially aid in managing particular types of chronic pain. While this area is currently under extensive investigation, it holds promising prospects for the future of pain management.
Nausea
GERD & Heartburn
Acid reflux occurs when stomach contents move back up into the oesophagus, leading to a condition known as GERD (Gastroesophageal Reflux Disease) if it happens frequently. GERD can result in esophagitis, characterized by inflammation or irritation of the oesophagus, although esophagitis is not always present in individuals with GERD. Common symptoms of GERD with esophagitis include heartburn, acid reflux, chest pain, nausea, and pain while swallowing. The precise cause of GERD is not always clear, but potential risk factors encompass the use of certain medications, obesity, exposure to secondhand smoke, pregnancy, and the presence of a hiatal hernia. Treatment for GERD may involve dietary modifications, smoking cessation, over-the-counter medications to alleviate symptoms, or targeted interventions addressing the underlying causes of the condition.
Leaky Gut Syndrome
The intestines harbour a diverse community of bacteria known as gut microbiota. These bacteria play crucial roles in digestion, safeguarding the intestinal wall, and supporting immune function. An imbalance in gut microbiota can adversely affect overall intestinal health, influencing factors like permeability. For instance, disruptions in gut microbiota balance can activate the body’s immune response, resulting in inflammation and heightened intestinal permeability (IP). These factors may contribute to leaky gut syndrome (LGS).
Tips To Improve Your Gut Health
Follow these guidelines to enhance your gut health:
- Engage in regular exercise to stimulate your colon and promote consistent bowel movements, aiding in the management of irritable bowel symptoms.
- Adopt a nutritious diet centred around fresh, unprocessed foods, as processed foods can quickly break down into sugars, negatively impacting digestive health.
- Opt for smaller, more frequent meals to prevent overwhelming the gastrointestinal tract.
- Thoroughly chew your food to facilitate the digestive process.
- Manage stress levels through activities like yoga, meditation, therapy, or journaling, as excessive stress can detrimentally affect gut health.
- Integrate probiotics into your diet through sources such as yogurt, kefir, fresh sauerkraut, or supplements to boost beneficial bacteria in your gut.
- Increase fiber intake to meet a daily goal of 25 grams.
- Stay adequately hydrated by consuming at least eight 8-ounce glasses of water daily.
- Restrict alcohol and caffeine intake, as both can act as digestive stimulants and disrupt the digestive process.
- Seek medical advice if you frequently experience diarrhea or constipation, as you may have irritable bowel syndrome, affecting 10 to 15 percent of the population. Trust your gut instincts, as your gut health directly impacts overall well-being.
Talk To a Doctor or Healthcare Professional
Comprising trillions of bacteria, fungi, and various microbes, your gut microbiome significantly influences health by regulating digestion and supporting the immune system, among other vital functions. An equilibrium between unhealthy and healthy microbes in the intestines is crucial, as an imbalance may be linked to issues such as weight gain, elevated blood sugar, high cholesterol, and various disorders. Seeking professional help will not only reduce your time of recovery but also give you a better chance of boosting your gut health.
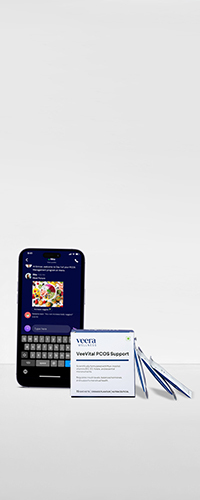
Learn More With Veera
Prioritizing a healthy gastrointestinal lifestyle is crucial for overall well-being and disease prevention. Focus on fiber, stay hydrated, include prebiotics and probiotics, exercise regularly, manage stress, maintain good hygiene, ensure sufficient sleep, and avoid smoking, alcohol, and processed foods. Following these guidelines enhances physical, mental, and emotional health, with support from Veera Health’s expert gynecologists.