Polycystic ovary syndrome presents various evident signs, such as irregular menstrual cycles, excessive facial or body hair growth, oily skin leading to acne, and weight gain. However, if you are unaware of your PCOS status, your breast discomfort could potentially serve as a subtle indicator. Women with PCOS are more prone to experiencing breast tenderness and retaining water. Therefore, if these symptoms resonate with you and conventional remedies have proven ineffective, it is advisable to seek a medical evaluation as a precautionary measure.
Understanding Polycystic Ovary Syndrome
While there is no definitive cure for PCOS, awareness of the condition is essential. Implementing positive lifestyle modifications can play a pivotal role in managing PCOS. Regular physical activity offers a multitude of advantages that extend beyond mere weight reduction for women with PCOS.
Weight management holds significant importance as it positively influences virtually all aspects of PCOS. Given that exercise is an effective calorie-burning activity, it can serve as a valuable tool in achieving and maintaining a healthy weight. Although PCOS can pose challenges to weight loss, even modest reductions, typically around five to ten percent of one’s body weight, can have a substantial impact on alleviating PCOS symptoms. Giving priority to physical activity can potentially enhance regular ovulation. When examining the relationship between exercise and PCOS, studies have shown that moderate-intensity physical activity has a positive impact on ovulation, and these improvements are not contingent on the specific type of exercise, its frequency, or the duration of each session.
Coping with the symptoms of PCOS can be emotionally taxing. Increasingly, research indicates that women with this condition are more susceptible to experiencing symptoms of depression. Engaging in regular exercise can prove beneficial for individuals dealing with mild to moderate depression and serves as an effective approach to enhancing one’s mood. During exercise, the body releases endorphins, which are hormones that foster a sense of well-being. This can assist in stress management and alleviate certain depressive symptoms.
Types of Breast Pain
Breast discomfort is a frequently encountered occurrence among women of all age groups. Experiencing painful, sensitive, or tender breasts can trigger significant apprehension. However, it’s important to note that breast pain, by itself, is typically not indicative of breast cancer.
For many women, breast pain is a normal part of their menstrual cycle, occurring in sync with their periods; this is referred to as cyclical breast pain. On the other hand, when breast pain persists outside of the menstrual cycle, it is categorized as noncyclical breast pain.
At times, discomfort that appears to originate in the breast may stem from another source, such as a strained muscle in the chest, a condition known as chest wall pain.
There are two fundamental categories of breast discomfort — cyclical and noncyclical.
Cyclical pain follows a pattern corresponding to your menstrual cycle. For instance, it might involve breast tenderness or pain occurring consistently at a specific point in your menstrual cycle. Many women encounter breast pain and tenderness roughly two weeks before the onset of their menstrual period. Cyclical pain is prevalent in approximately 75 percent of cases and primarily affects women aged 20 to 50. It typically resolves after menopause. This type of breast pain tends to manifest in the upper and outer regions of both breasts and may also extend to the underarm area.
Noncyclical pain, in contrast, is not linked to the menstrual cycle and does not exhibit a predictable recurring pattern. Typically, postmenopausal women between the ages of 40 and 50 experience noncyclical breast pain. This kind of discomfort is often described as a sensation of tightness, a burning feeling, or general breast soreness. It can persist either continuously or intermittently.
What Are the Causes?
- Hormonal fluctuations are responsible for breast soreness.
The primary cause of breast pain in women is hormonal changes. Typically, breasts become tender or sore in the three to five days leading up to the start of the menstrual period, with the discomfort subsiding once menstruation begins. This occurrence is attributed to an increase in estrogen and progesterone levels just before the onset of the menstrual cycle. These hormones prompt breast swelling and can result in tenderness.
It’s perfectly normal to experience occasional breast tenderness around the time of your menstrual period, and there’s generally no cause for concern.
During early pregnancy, breast soreness can persist throughout the first trimester as hormonal production increases. For many women, breast tenderness serves as one of the initial indicators of pregnancy.
2. You’ve sustained a breast injury
Similar to any other part of your body, the breasts are susceptible to injury. Such injuries can occur as a result of accidents, sports-related incidents, or even breast surgery. At the moment of the injury, you might experience sharp, shooting pain. Following the trauma to the breast, tenderness can persist for several days or even weeks. It is advisable to consult your doctor if the pain does not alleviate or if you observe any of these symptoms:
- Pronounced swelling
- The presence of a breast lump
- Redness and warmth, which could indicate an infection
- A persistent bruise on your breast
3. Your breast discomfort may be caused by an ill-fitting bra
In the absence of adequate support, the ligaments that link the breasts to the chest wall can experience excessive stretching, leading to discomfort and soreness by the day’s end. This discomfort may become particularly evident during physical activities. Ensuring that your bra is the right size and offers proper support is crucial to address this issue.
4. The source of your discomfort may be the chest wall, not the breasts
What you perceive as breast pain might originate from your chest wall — an anatomical region composed of muscle, tissue, and bone that envelops and shields your heart and lungs. Typical causes of chest wall pain encompass:
- Strained or pulled muscle
- Inflammation in the vicinity of the ribs
- Chest wall trauma (such as a blow to the chest)
- Fractured bone
5. Breast tenderness can result from breastfeeding
Breastfeeding can occasionally lead to breast discomfort. Some of the sensations and issues you may encounter while nursing include:
- Nipple pain stemming from an incorrect latch (how the baby attaches to the breast for feeding)
- A tingling sensation during letdown (when milk begins to flow to the baby)
- Nipple soreness caused by biting, dryness, cracked skin, or an infection
6. You’re experiencing a breast infection
Breast infections, known as mastitis, are more commonly encountered by breastfeeding women but can occasionally affect others as well. If you have a breast infection, you may exhibit symptoms in one breast, such as:
- Pain
- Redness
- Swelling
- Fever
7. Breast pain may potentially result from medication side effects
Certain medications have the potential to induce breast pain as an adverse reaction. It is advisable to consult your healthcare provider regarding the medications you are currently taking and whether this could be a contributing factor in your case. Some drugs associated with this recognized side effect include:
- Oxymetholone is employed in the treatment of certain forms of anemia.
- Chlorpromazine is prescribed for various mental health conditions.
- Diuretics (water pills) are medications that promote increased urination and are used to manage kidney and heart conditions, as well as high blood pressure.
- Hormone therapies encompass birth control pills, hormone replacement therapies, and infertility treatments.
- Digitalis is prescribed for the treatment of heart failure.
- Methyldopa is used to manage high blood pressure.
8. You may be dealing with a painful breast cyst
If you notice a tender lump suddenly appearing in your breast, it could be indicative of a cyst. These fluid-filled lumps are typically benign and may often resolve without the need for treatment. However, it is essential to have any breast lump assessed by a medical professional.
To confirm a cyst, your doctor might recommend a mammogram, ultrasound, or aspiration (removing fluid from the lump). Draining the cyst’s fluid is also a therapeutic option. In cases where the cyst isn’t causing significant discomfort, treatment may not be necessary.
9. You’re experiencing discomfort associated with breast implants
Some women encounter complications related to breast implants, whether they are composed of silicone or saline. A common cause of pain following breast augmentation surgery is capsular contracture, where scar tissue tightens around the implants. Breast pain can also indicate a potential rupture of one of the implants. To determine if your breast pain is linked to your breast implants, it’s advisable to consult your healthcare provider.
10. Breast pain can occasionally serve as an indicator of breast cancer
Although breast cancer is not commonly associated with pain, it is not impossible. Inflammatory breast cancer, while rare, is an exception, accounting for 1% to 5% of breast cancer cases in the United States. Symptoms of this aggressive form of cancer tend to manifest suddenly and progress swiftly. Inflammatory breast cancer may lead to the breast becoming:
- Red or discolored
- Swollen or heavy
- Painful
What Are the Symptoms?
Cyclic breast pain
- Linked to the menstrual cycle and hormonal fluctuations
- Characterized as a sensation of dullness, heaviness, or aching
- Frequently accompanied by breast swelling, a sense of fullness, or the presence of lumpiness
- Typically impacts both breasts, particularly affecting the upper and outer regions, with potential radiating discomfort extending toward the underarm
- Escalates during the two weeks leading up to the onset of the menstrual period and subsequently diminishes
- More commonly experienced by individuals in their 20s and 30s, as well as those in their 40s who are undergoing the transition to menopause
Noncyclic breast pain
- Not associated with the menstrual cycle
- Characterized by sensations of tightness, burning, stabbing, or aching
- Persistently present or occurring intermittently
- Typically confined to a specific area in one breast, although it may occasionally spread more broadly across the breast
- More commonly observed in women, especially postmenopause
The Link Between Hormones and Breast Tenderness
Breast tenderness or swelling is typically associated with hormonal fluctuations preceding menstruation. This type of breast discomfort often results in tenderness in both breasts and may extend to the underarm area.
When breast pain is tied to the menstrual cycle, it is referred to as cyclic breast pain. Cyclic breast pain can be one component of a cluster of symptoms that emerge before menstruation, known as premenstrual syndrome (PMS), or it may manifest independently.
Additional symptoms of PMS include:
- Mood swings
- Acne
- Headaches
- Bloating
- Diarrhea or constipation
- Fatigue
- Sleep disturbances
PMS is temporary and typically subsides a few days after the onset of menstruation. During this time, individuals can alleviate symptoms by using over-the-counter (OTC) pain relievers, donning a comfortable and supportive bra, and applying gentle heat to alleviate discomfort.
Breast pain can also arise due to other hormonal shifts, such as those occurring during pregnancy or the initial stages of menopause.
Tips for Managing PCOS-Related Breast Pain
The choice of treatment will be contingent upon whether you are experiencing cyclical or noncyclical breast pain. Before prescribing a treatment plan, a healthcare provider will consider factors such as your age, medical history, and the intensity of your discomfort.
For cyclical pain, treatment options may encompass:
- Wearing a supportive bra.
- Reducing your sodium and caffeine intake.
- Using oral contraceptives can help regulate hormone levels.
- Administering estrogen blockers, such as tamoxifen.
- Taking pain-relieving medications, including nonsteroidal anti-inflammatory drugs like ibuprofen.
It’s important to always consult with a healthcare provider before introducing any supplements, ensuring they won’t interfere with your current medications or exacerbate other health conditions.
Consult a Doctor for Preventative Care
Schedule a consultation with your healthcare provider if you experience breast pain under the following circumstances:
- Persists continuously for over a few weeks.
- Manifests in a specific, localized area of your breast.
- Appears to be worsening progressively.
- Impedes your daily routines and activities.
- Disrupts your sleep, causing you to awaken during the night.
It’s worth noting that the risk of breast cancer is typically very low in individuals whose primary symptom is breast pain. Nonetheless, if your healthcare provider advises an evaluation, it is crucial to heed their recommendation.
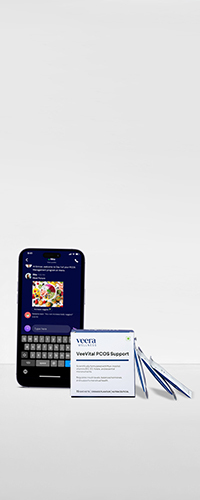
Learn More With Veera
There are various other symptoms of PCOS apart from breast pain and some of them are so rare that you might misdiagnose them. This is why experts at Veera Health consult with their clients with utmost attention, no judgment and concentration on minute details. Begging your journey of PCOS reversal with India’s largest PCOS platform.