[vc_row][vc_column][vc_column_text woodmart_inline=”no” text_larger=”no”]
[/vc_column_text][/vc_column][/vc_row][vc_row][vc_column][vc_column_text]
How PCOS affects your body?
[/vc_column_text][vc_column_text]
Ovulation is the process of the release of an egg from the ovary which normally occurs once a month (usually the 13th or 14th day of a 28 day cycle). The egg matures in the ovary within a follicle (fluid filled sac). Although each month there are several follicles that develop, usually only one develops fully and the egg within that follicle is released from the ovary. The egg then travels to the fallopian tube to get fertilised if sexual intercourse has taken place at the time of ovulation, and the new embryo can then implant in the uterus, resulting in pregnancy.
Now, in women with PCOS, ovulation may not occur every month, which means the egg is not released on a regular basis. Ovulation can either entirely stop (anovulation) or occur irregularly (oligo-ovulation). This makes it difficult for women with PCOS to get pregnant because either there is no egg released to undergo fertilisation.[/vc_column_text][/vc_column][/vc_row][vc_row][vc_column][vc_column_text]
PCOS and long-term health complications
[/vc_column_text][vc_column_text]
Getting pregnant and carrying that pregnancy through all the trimesters is a complex process that requires a balance of many different hormones. In PCOS, however, the ovaries produce higher than normal levels of androgens (male hormones), which causes hormonal imbalance. The presence of high levels of androgens interferes with the normal cycle of ovulation (egg release) and menstruation. As a result, many fluid-filled sacs called follicles do not mature and hence do not release an egg. These follicles are the “cysts” you see on your ultrasound scan, though this term is inaccurate.
[/vc_column_text][vc_column_text]
Although women usually do recover from gestational diabetes after the baby is born, it can still put them at a higher risk of developing type 2 diabetes later in their lives. Pre-eclampsia, another pregnancy complication, is the sudden increase in blood pressure that is dangerous for the mother and the baby’s health. The risk of developing such complications makes it very important to have your pregnancy closely monitored by your doctor for a healthy term.
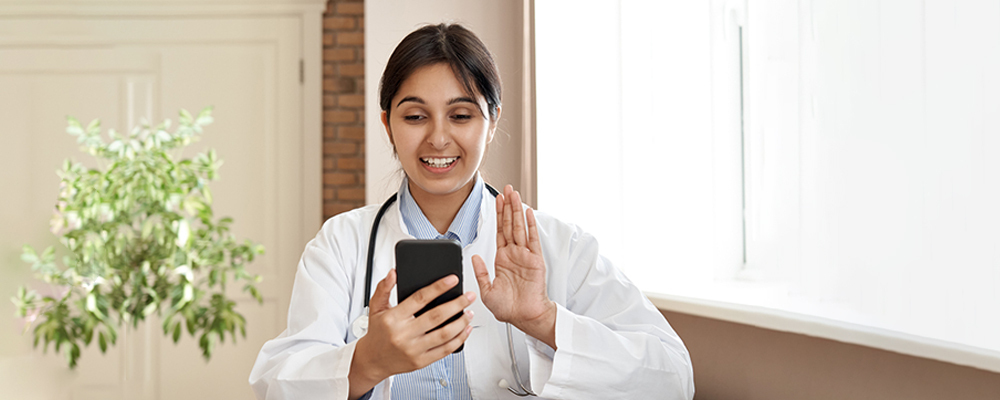
If you’re diagnosed with PCOS and are finding it difficult to get pregnant — you’re not alone. While PCOS does affect certain processes in your body that make it harder to get and stay pregnant, there are plenty of treatment options available. Speaking to your doctor is the first step in finding out what you can do to improve your chances of conceiving and successfully carrying a pregnancy to term.
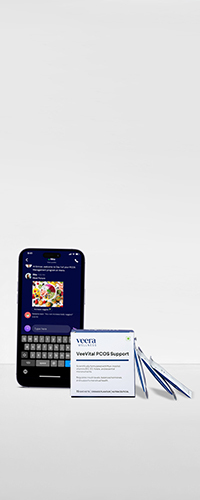
At Veera Health, we provide you with the guidance and support you will need to successfully conceive – book your free appointment today![/vc_column_text][/vc_column][/vc_row][vc_row][vc_column][vc_column_text]
How can you reduce the risk of developing long-term complications?
[/vc_column_text][vc_column_text]Lifestyle changes: For overweight PCOS patients, losing even 5%-10% of body weight is shown to help regularize periods and ovulation, which increases the chances of getting pregnant. Making lifestyle changes includes following a healthy, balanced diet combined with regular physical activity. In fact, making lifestyle changes is the first line of treatment in improving the symptoms of PCOS.
Medications: While lifestyle changes do help, for some women medications are required to help induce ovulation. Letrozole is a widely used treatment for infertility in women with PCOS and has been shown to be more effective than other medications such as clomiphene citrate. Other medications such as metformin and gonadotropins can also help induce ovulation.
Tracking ovulation: Since most women with PCOS have irregular periods, it can get difficult to estimate your ovulation time. There are several physical signs you can track to monitor your ovulation — such as mucus changes (classically “egg white” slippery clear mucus just before ovulation) and basal body temperature (periovulatory temperature should rise slightly) Additionally, there are ovulation kits available in the market that can help you track ovulation. By tracking your ovulation, you can accordingly plan to have sexual intercourse around the days of ovulation. However, ovulation predictor kits are often not accurate in women with PCOS, so these should be interpreted with caution.
Assisted reproductive technology: For women who have not found luck conceiving naturally or by using a combination of lifestyle modifications and medications to improve their fertility, assisted reproductive technology is another option. This includes treatments such as IVF (in vitro fertilisation). Since these procedures are expensive and demanding, it is often the last option after having tried other less intensive treatments.[/vc_column_text][/vc_column][/vc_row][vc_row][vc_column][vc_column_text woodmart_inline=”no” text_larger=”no”]Disclaimer: Content on Veera is provided for informational purposes only and is not intended as medical advice, or as a substitute for medical advice given by a physician[/vc_column_text][/vc_column][/vc_row]