Bloating is a common experience that can affect anyone intermittently, often triggered by factors such as excessive sugar consumption, large meals, or bouts of anxiety. However, if you frequently find yourself dealing with bloating, it could be linked to Polycystic Ovary Syndrome (PCOS). Women with PCOS are more prone to experiencing bloating, yet many are unaware of the connection between their condition and this discomfort. This lack of awareness often leads them to attribute the issue to their dietary choices. While diet is certainly a contributing factor, it’s not the sole explanation for the prevalence of bloating among women with PCOS.
Within your gastrointestinal system resides a vast community of approximately 100 trillion bacteria, which can be categorized into three groups: beneficial bacteria, neutral bacteria and harmful bacteria. Under ideal conditions, your body maintains a delicate equilibrium among these three categories to optimize its functions and stave off diseases. However, various factors, such as your dietary choices, antibiotic usage and environmental influences, can disrupt this balance, leading to a condition referred to as dysbiosis.
Dysbiosis emerges when an imbalance of bacteria occurs within your gut. This imbalance may involve an overabundance of detrimental bacteria, a deficiency of beneficial bacteria, or a lack of bacterial diversity. Regrettably, individuals with PCOS, particularly women, are more susceptible to experiencing dysbiosis compared to those without the condition.
Dysbiosis serves as a significant underlying cause of abdominal bloating in PCOS. Furthermore, dysbiosis can exacerbate other PCOS symptoms, including acne, unwanted hair growth, hair loss and hormonal imbalances.
PCOS Overview
Polycystic ovarian syndrome (PCOS) is a prevalent hormonal disorder that impacts as many as one in every ten women during their reproductive years. It can lead to irregularities in the menstrual cycle, alterations in skin and hair and the development of ovarian cysts.
Remarkably, despite being a leading contributor to infertility, numerous individuals are unaware of their PCOS status, and many females with the condition remain undiagnosed. While PCOS is not curable, if you have it, you and your healthcare provider can collaborate to manage and effectively address its effects.
What Causes Gas?
Gas typically enters your digestive system through the intake of air during swallowing or when bacteria in the large intestine break down undigested carbohydrates. Increased gas symptoms may occur if there is a higher intake of air or consumption of specific foods and beverages.
Air Ingestion:
During eating and drinking, everyone naturally swallows a small amount of air. If the swallowed air doesn’t exit the stomach through belching, it may move into the intestines and eventually be expelled through the anus. Factors contributing to increased air intake and, consequently, more gas symptoms include:
- Chewing gum or sucking on hard candy
- Drinking carbonated or fizzy beverages
- Eating or drinking too quickly
- Smoking
- Wearing loose-fitting dentures
Bacteria in the Large Intestine:
The large intestine harbors a substantial number of bacteria, along with some fungi and viruses, collectively forming the gut microbiome. These microorganisms play a vital role in digestion. Bacteria in the large intestine assist in breaking down carbohydrates, generating gas in the process.
Certain foods and beverages contain carbohydrates, such as sugars, starches and fiber, that the stomach and small intestine do not completely digest. Undigested carbohydrates proceed to the large intestine, where bacteria break them down, resulting in the production of gas. Increased consumption of carbohydrates that are not fully digested by the stomach and small intestine may lead to heightened gas symptoms.
What Causes Bloating?
Abdominal bloating is a common occurrence, often recurring in a familiar pattern for many individuals. Generally, when bloating follows a predictable course, it is not a cause for concern. However, alterations in this pattern or an intensification of bloating beyond the expected level may indicate various conditions:
Gas:
A prevalent cause of bloating is the accumulation of gas in the stomach and intestines. Associated symptoms may include frequent burping, excessive gas passage, sudden urges to pass stool and a sense of nausea. Bloating from gas can range from mild discomfort to severe pain, with some individuals describing a feeling of something being trapped in their stomach. Potential causes of gas include certain foods (carbonated beverages, dairy, beans, cauliflower, broccoli and cabbage), swallowing air while eating or chewing gum, stomach infections and chronic illnesses like celiac disease or irritable bowel syndrome (gastrointestinal problems). Typically, gas symptoms subside on their own after a few hours.
Indigestion:
Indigestion, also known as dyspepsia, manifests as stomach discomfort or pain, sometimes accompanied by bloating. Common triggers for indigestion episodes include overeating, excessive alcohol consumption, taking stomach-irritating medications (such as ibuprofen), or minor stomach infections. Persistent indigestion with unexplained bloating not linked to food or apparent causes may be indicative of more serious conditions like a stomach ulcer or stomach cancer.
Infection:
Stomach infections can lead to bloating, often accompanied by diarrhea, vomiting, nausea and stomach pain. Bacterial infections (e.g., Escherichia coli or Helicobacter pylori) or viral infections (e.g., norovirus or rotavirus) may be responsible. While some infections resolve on their own within a few days, persistent symptoms lasting over a week may warrant medical attention, especially if accompanied by fever, bloody stool, or severe and frequent vomiting.
Small Intestinal Bacterial Overgrowth (SIBO):
An imbalance in the bacterial composition of the small intestine, termed SIBO, can cause bloating, frequent diarrhea and difficulties in digesting food. Chronic symptoms may lead to complications such as osteoporosis, metabolic bone disease, or weight loss.
Fluid Retention:
Factors like salty foods, hormonal changes and food intolerances can lead to increased fluid retention, causing bloating. Chronic bloating due to fluid retention might signal underlying issues like liver or kidney failure or diabetes.
Food Intolerances:
Bloating after consuming specific foods is common in individuals with lactose intolerance, gluten intolerance, or celiac disease. Eliminating the problematic foods usually resolves bloating.
Chronic Disorders:
Conditions like irritable bowel disease (IBD) and irritable bowel syndrome (gastrointestinal problems) can contribute to bloating, with symptoms such as gas, diarrhea and vomiting. Unexplained weight loss may indicate a more serious condition like Crohn’s disease.
Gastroparesis:
Gastroparesis, a disorder affecting normal stomach emptying, can cause bloating along with symptoms like constipation, early satiety, heartburn, nausea and vomiting. Diseases such as diabetes or hypothyroidism, as well as certain gastrointestinal surgeries, can contribute to gastroparesis.
Gynecological Disorders:
Some gynecological issues, including menstruation, menopause and endometriosis, can lead to bloating. Bloating may also be a symptom of early ovarian cancer in women, along with weight gain, constipation and pain.
Constipation:
Bloating may arise from constipation, where food accumulates in the gut. Causes include dehydration, insufficient dietary fiber, food intolerance, pregnancy, certain bowel disorders, nutrient deficiencies and certain medications. Lifestyle adjustments, including increased water intake, dietary changes, exercise, or the use of laxatives, can often alleviate constipation and associated bloating.
The Connection Between PCOS and Digestive Issues
Gastrointestinal Symptoms
1) Hormonal Influence:
PCOS is exclusive to women, whereas gastrointestinal problems disproportionately affect twice as many women as men. In PCOS irregular menstrual cycles arise due to altered LH: FSH ratio, not allowing ovulation to happen This study also suggests a potential link between these hormones and gastrointestinal problems, as excess FSH and LH may induce constipation by delaying the movement of food in the digestive system. Elevated perceptions of pain may be associated with female sex hormones.
2) Inflammation and Impact on Life Quality:
Both PCOS and gastrointestinal problems significantly impact the quality of life for affected individuals. Additionally, they share common symptoms such as bloating, abdominal pain and changes in bowel habits, all stemming from inflammation. Chronic inflammation, a characteristic feature of both conditions, results in internal cellular stress and external environmental stress. In the case of PCOS, there is an increased risk of inflammatory issues such as insulin resistance, type 2 diabetes mellitus, obesity, cholesterol problems and heart-related complications. Symptoms of depression and anxiety may also manifest in individuals with both gastrointestinal problems and PCOS, attributed to the intricate connection between the gut and the brain.
3) Intestinal Permeability:
Recent studies establish a connection between PCOS and both intestinal permeability and alterations in gut bacteria. Enhanced intestinal permeability, commonly known as leaky gut, is a well-documented factor contributing to gastrointestinal problems. To simplify, this condition involves the gradual degradation of the protective mucosal barrier in the intestines, leading to the formation of “holes.” Similar to a compromised water hose, these holes allow toxins and inflammatory substances to leak into the bloodstream, triggering symptoms. This is when noticeable manifestations of both PCOS and gastrointestinal problems tend to emerge.
Insulin Resistance
Insulin resistance constitutes a significant characteristic present in both individuals with obese and lean PCOS. This condition manifests in 70-95% of those with obese PCOS and 30-75% of individuals with lean PCOS.
Importantly, high insulin levels not only serve as a symptom but also play a pivotal role in driving the development of PCOS. Elevated insulin levels have the potential to hinder ovulation and prompt the ovaries to produce excessive amounts of testosterone.
A research study noted a notable correlation between the increasing prevalence of PCOS and the rise in obesity and weight gain over the past decade. Another scholarly article highlighted a discernible surge in PCOS, described as a “galloping increase,” aligning with the escalating prevalence of type 2 diabetes.
Managing Gas and Bloating in PCOS
Polycystic Ovary Syndrome (PCOS) can often come with gastrointestinal symptoms that may include bloating, indigestion and irregular bowel movements. Managing these symptoms is essential for your overall well-being.
Medical Approaches
Holistic Approaches
Here are some tips to help you manage PCOS and its associated gastrointestinal symptoms:
- Balanced Diet: Follow a well-balanced diet that includes whole grains, lean proteins and plenty of fruits and vegetables. Avoid excessive consumption of processed foods and sugars, as they can exacerbate both PCOS and gastrointestinal discomfort.
- Fibre-Rich Foods: Increase your intake of fiber-rich foods like whole grains, legumes and vegetables. Fibre can help regulate your bowel movements and reduce bloating.
- Hydration: Drink plenty of water throughout the day to help with digestion and prevent constipation. Proper hydration can also alleviate bloating.
- Regular Meals: Eat regular meals and avoid skipping them. This can help stabilize your blood sugar levels, which is crucial for managing PCOS symptoms.
- Mindful Eating: Practise mindful eating, which involves paying close attention to your body’s hunger and fullness cues. This can help prevent overeating and indigestion.
- Low-Glycemic Index (GI) Foods: Incorporate low-GI foods into your diet. They can help regulate blood sugar levels and may alleviate some PCOS symptoms.
- Probiotics: Consider adding probiotics to your diet in the form of yogurt, kefir, or supplements. Probiotics can promote a healthy gut and aid digestion.
- Regular Exercise: Engage in regular physical activity. Exercise can help regulate hormones, improve insulin sensitivity and alleviate PCOS symptoms, including gastrointestinal discomfort.
- Stress Management: Practice stress-reduction techniques like meditation, yoga, or deep breathing exercises. High stress levels can exacerbate gastrointestinal issues and PCOS symptoms.
- Medication and Supplements: Consult with a healthcare provider to discuss the potential use of medications or supplements for specific gastrointestinal symptoms. They can provide guidance based on your individual needs.
- Monitor Food Sensitivities: Keep track of how your body reacts to different foods. Some individuals with PCOS may have food sensitivities that can trigger gastrointestinal discomfort. Identifying and avoiding these trigger foods can be helpful.
- Consult a Specialist: If your gastrointestinal symptoms are severe or persistent, consult a gastroenterologist to rule out other underlying gastrointestinal conditions and get tailored treatment recommendations.
Consult a PCOS Doctor
If gas and bloating are accompanied by additional symptoms, it may signal an underlying issue beyond normal digestive processes. It is advisable to consult a physician if you experience gas and bloating in conjunction with any of the following:
- Presence of blood or mucus in your stool
- Unsuccessful results from changes in your dietary habits
- Persistent or recurrent occurrences of diarrhea, constipation, or vomiting
- Development of a fever
- Loss of appetite
- Ineffectiveness of over-the-counter remedies
- Sustained and uncomfortable bloating, gas, or heartburn
- Significant alterations in bowel movements
- Symptoms that are negatively impacting your daily life
- Unexplained weight loss
When you seek medical attention, your doctor will likely initiate the process by discussing your medical history and a detailed account of your symptoms. Maintaining a symptom journal can be beneficial, recording information such as circumstances, food consumption, symptom intensity and factors that alleviate or exacerbate the symptoms. A physical examination of your abdomen will be conducted by your physician to identify any abnormalities or tenderness.
Based on the findings and your medical history, your doctor may suggest various diagnostic tests, such as a colonoscopy, blood tests, upper gastrointestinal imaging, or breath tests, to ascertain the underlying cause of your symptoms.
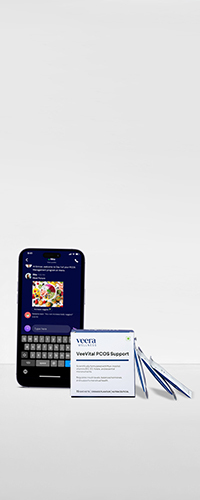
Learn More With Veera
Dietitians and care managers at Veera Health constantly strive to make your PCOS journey effective and customized. They will guide you with meal plans that help with gas and bloating and all you have to do is take this simple diet quiz and win a free diet consultation with a nutritionist.