When you think about the PCOS problem, you first think about irregular periods or trouble conceiving. But have you thought about PCOS leading to diabetes?
Polycystic ovary syndrome or PCOS does not outright cause diabetes but if PCOS is left untreated, it can increase the risk of developing 2 diabetes in the future. However, you can manage PCOS and prevent the development of such complications
Link Between PCOS and Diabetes
Insulin resistance is one of the drivers of PCOS in women. Having insulin resistance not only worsens PCOS symptoms but also increases your risk of developing many health problems in the future. Although PCOS and diabetes are not directly linked, having PCOS does put you at risk of developing type 2 diabetes if the insulin resistance is left untreated. Progression to diabetes can happen gradually, as the levels of blood glucose levels keep increasing with insulin not being able to effectively move the glucose in the cells. Being overweight worsens the risk of insulin resistance, however, even lean women with PCOS are also at risk of being insulin resistant with PCOS.
Signs and Symptoms of Insulin Resistance PCOS
The signs of insulin resistance can be subtle, and you may or may not see obvious changes. This makes it important to test for insulin resistance and keep your blood glucose levels in check. However, there are certain signs that can indicate insulin resistance:
- Trouble losing weight or unexplained weight gain
- Fatigue
- Cravings
- Headache
- Dark skin patches in skin folds
How Does PCOS Cause Diabetes and Prediabetes
In type 2 diabetes, a person is still able to produce insulin but How and how well insulin works to manage blood glucose is what determines the level of insulin resistance:8
- Functioning Normally: The pancreas is able to produce the required amount of insulin as needed to help glucose enter cells in the muscle, fat, and liver cells, which will be then used for energy.
- Insulin resistance: The cells stop responding as properly to insulin. As a result, the pancreas releases extra insulin to make up for the cells’ inability to take up glucose. This causes high insulin levels in the blood
- Prediabetes: The cells are still not responsive to insulin, and the pancreas is not able to create enough insulin to keep blood sugar levels stable. Extra glucose remains in the blood and blood sugar levels is higher than normal, but not high enough to be diagnosed with diabetes
- Type 2 Diabetes: This stage usually occurs after prediabetes if blood sugar is not kept in control. Blood sugar levels are much higher in diabetes than in prediabetes, and the risk of complications also increases
One stage does not always have to progress to another if proper management and treatment have taken place. If left untreated, women with PCOS can progress from insulin resistance to prediabetes and to type 2 diabetes. However, the good news is, that there are plenty of treatment options to reduce the chances of progression and even reverse prediabetes.
PCOS and Gestational Diabetes
Insulin resistance is one of the common causes of PCOS and is responsible for many symptoms of PCOS. Having untreated insulin resistance can put you at an increased risk of developing gestational diabetes i.e. diabetes during pregnancy. The risk of developing gestational diabetes is higher in overweight women.
PCOS pregnancy can come with many complications that can affect both the mother and the baby’s health. Most women recover from gestational diabetes after they’ve given birth and after their blood glucose levels have normalized. However, they may still be at risk of developing type 2 diabetes later in life if they don’t continue to follow a healthy lifestyle. Eating the right foods, and exercising regularly during and after pregnancy can help reduce this risk.
Is it Possible to Manage one Disorder while Managing the Other?
Yes, you can manage PCOS and insulin resistance or type 2 diabetes together. Your PCOS treatment needs to be customized to your symptoms and concerns so your doctor can help you come up with a plan that best suits your needs. In fact, when you manage insulin resistance properly, you’ll observe that many symptoms of PCOS such as weight gain, irregular periods, and weight gain, start to also improve.
How to Reverse Insulin Resistance PCOS
You can put your diabetes into remission and manage your PCOS symptoms by following a healthy lifestyle. If you are already insulin resistant, you can prevent the progression to type 2 diabetes by first managing your lifestyle and taking medications where required.
PCOS and Diabetes Diet
A diet that is balanced, nutritious, and rich in whole foods instead of processed and packaged can help maintain blood glucose levels. Usually, low glycemic index carbohydrates such as brown rice, millets, quinoa, and steel-cut oats can help release glucose slowly in the blood. Along with carbohydrates, having quality protein, healthy fats, and dietary fiber is also important.
Lifestyle
Making the required lifestyle changes include eating a balanced, healthy diet, exercising regularly, managing stress levels, and getting good quality sleep is an important part of managing the hormonal imbalance and keeping insulin resistance in check.
Exercise and Yoga
Apart from diet, doing regular PCOS exercise is the best way to improve insulin resistance and lose weight. Although any kind of activity that you enjoy performing is good for PCOS, a combination of cardio and strength training works the best by increasing lean muscle mass and increasing insulin sensitivity.
PCOS and Diabetes Treatment
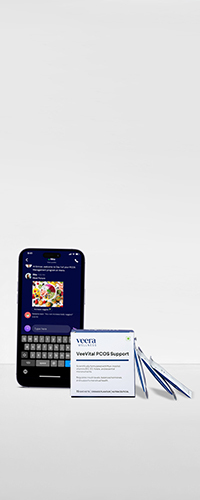
Apart from lifestyle changes, medications can also be an important part of your PCOS treatment plan. Drugs such as metformin can help improve insulin sensitivity thereby decreasing insulin resistance and reducing the symptoms of PCOS.
How do Diabetes and PCOS Affect Pregnancy?
Having high glucose levels in the blood can be harmful to your baby’s development. This is because your baby starts to develop many vital organs during the first trimester such as the brain, kidney, heart, and lungs and high glucose levels can increase the risk of birth defects such as heart or brain defects. High blood glucose can also increase the risk of having a miscarriage or a stillborn baby. Apart from these, your baby may also develop breathing problems or way too or be born preterm, or have low blood glucose after birth.
For the mother, pregnancy can worsen some of the long-term complications of diabetes such as kidney or eye problems. There is also a risk of developing preeclampsia (sudden increase in blood pressure) which can be dangerous for both the mother and the baby.
Conclusion
PCOS and diabetes are both chronic conditions that can affect many areas of your health. However, you can manage both these conditions with proper lifestyle management and medications where required. If you have insulin resistance, with effective and early management you can prevent its progression to type 2 diabetes. The sooner you develop healthy lifestyle habits, the better the health outcomes.