Polycystic Ovary Syndrome (PCOS) stands apart from autoimmune conditions, yet it does show a delicate connection with the immune system. PCOS manifests as a complex hormonal irregularity, marked mainly by imbalanced hormones. It is followed by unpredictable menstrual patterns and the development of small ovarian cysts. It is commonly believed to be influenced by a mix of genetic, hormonal, and environmental factors.
Notably, studies do suggest a possible connection between PCOS and the immune system. Heightened levels of specific inflammatory indicators have been detected in the bloodstream of individuals with PCOS. This persistent, chronic inflammatory state could potentially contribute to the emergence of insulin resistance and other metabolic challenges. It is, however, imperative to underscore that the intricate mechanisms governing these correlations continue to be subjects of investigation.
What is PCOS?
Polycystic Ovary Syndrome (PCOS) is a prevalent hormonal imbalance condition impacting women. It showcases a mix of symptoms, including irregular menstrual patterns, surplus production of androgen (male hormone), and insulin resistance, which thus affects the metabolism. These hormonal discrepancies give rise to an array of bodily and psychological symptoms.
A defining attribute of PCOS lies in its repercussions on reproductive well-being. The irregularity or absence of menstruation can pose challenges for PCOS-affected individuals aiming for conception. PCOS thereby acts as a primary contributor to infertility.
Given its multifaceted nature, PCOS requires a comprehensive and individualized approach to its management, which may include lifestyle modifications, hormonal therapy, and addressing associated health risks.
What are autoimmune diseases?
Normally, our immune system guards the body against harmful things like viruses and bacteria. But sometimes, it starts attacking healthy cells, tissues and organs. This confusion happens because the immune system can’t tell the difference between our cells and outside cells. Instead of protecting us, it causes problems like inflammation, hurting our tissues and causing different symptoms.
Health issues connected to the immune system can impact different body parts, causing various complications. Various problems such as rheumatoid arthritis, type 1 diabetes, multiple sclerosis, lupus and celiac disease are included in this category. There are over 80 recognized immune-related diseases, each impacting different body parts and causing various problems.
The link between PCOS and Autoimmune Disorders
The interrelation between Polycystic Ovary Syndrome (PCOS) and autoimmune aspects is gaining traction within medical circles. Although PCOS is not officially categorized as an autoimmune disorder, emerging research suggests potential correlations between PCOS and shifts in the immune system’s operation.
Autoimmune conditions entail the immune system erroneously targeting the body’s tissues. In contrast, PCOS is chiefly marked by irregular hormonal patterns and reproductive challenges. However, shared genetic factors and immune system involvement in both conditions have spurred investigations into potential connections.
Certain inquiries have suggested a potential increase in the occurrence of specific autoimmune conditions, such as Hashimoto’s thyroiditis or autoimmune thyroid disease, among those affected by PCOS. Moreover, the presence of chronic, subdued inflammation — often observed in PCOS — mirrors a defining characteristic of several autoimmune disorders.
This inflammation can exacerbate the prevailing insulin resistance and metabolic disturbances that are common in PCOS. Furthermore, elevated levels of cytokines, pivotal components of the immune response, have been identified in women with PCOS. These cytokines could potentially contribute to the emergence of insulin resistance and hormonal irregularities synonymous with PCOS.
Important factors to consider
When exploring the link between PCOS and autoimmune disorders, several important factors are seen, shedding light on the complex interplay between these two realms of health.
Both PCOS and autoimmune conditions might share a genetic underpinning, and these common genetic elements could potentially heighten vulnerability to both ailments in specific individuals. Hormonal imbalances are a definitive trait of PCOS, and these imbalances could potentially exert an influence on immune reactions and foster the onset of autoimmune responses.
In addition, the role of inflammation emerges as a pivotal link connecting PCOS and autoimmune conditions. Prolonged inflammation is a recurring trait in several autoimmune disorders and has also been witnessed in individuals grappling with PCOS. This inflammatory backdrop might act as a catalyst for some of the metabolic discrepancies and insulin resistance observed in PCOS.
Hormonal factors
Hormonal factors play a central role in both Polycystic Ovary Syndrome (PCOS) and autoimmune disorders, contributing to the complex relationship between these two health domains.
In PCOS heightened levels of androgens, encompassing testosterone, have the potential to disturb the customary menstrual cycle, resulting in irregular periods, excessive hair growth known as hirsutism and the occurrence of acne.
Furthermore, the presence of insulin resistance, frequently linked to PCOS, could potentially intensify the generation of androgens. These hormonal irregularities are not only responsible for the reproductive symptoms of PCOS but may also interact with the immune system. Androgens can influence immune cell function, potentially contributing to immune system dysregulation.
Similarly, in autoimmune disorders, hormonal factors can influence disease progression and symptom severity. By delving into these connections, researchers and healthcare professionals aim to uncover potential therapeutic avenues. These avenues could offer relief and improved management for those affected by these complex health challenges.
Inflammation
The role of inflammation assumes significance within the domain of Polycystic Ovary Syndrome (PCOS), adding to the intricate character of the condition. Ongoing investigations have illuminated the presence of persistent, chronic inflammation in those affected by PCOS, thereby shedding light on the fundamental mechanisms and potential health implications.
The genesis of this observed inflammation in PCOS is thought to be varied, arising from factors like dysfunction within adipose tissue, insulin resistance and imbalances in hormones. This prolonged inflammation possesses the capability to worsen the metabolic upheavals frequently associated with PCOS, which encompass insulin resistance and obesity. Consequently, these metabolic alterations might further accentuate inflammation, creating a cycle that contributes to the emergence and advancement of the syndrome.
Genetic predisposition
PCOS, or Polycystic Ovary Syndrome, is an intricate and multifaceted condition that engages numerous biological pathways. While it isn’t categorized as an autoimmune ailment, data is proposing a hereditary inclination toward PCOS. Genetic components seem implicated in PCOS progression since the disorder frequently recurs in families. Specific genetic deviations and changes have been pinpointed, possibly adding to the hormone imbalances and metabolic irregularities observable in PCOS. These genetic elements, together with outside influences, could contribute to the heterogeneous character of the syndrome. Nonetheless, the precise interplay between genetics and other aspects of PCOS is a lively domain of exploration.
Environmental triggers
The focus has shifted toward environmental factors as potential influencers in the initiation and progression of Polycystic Ovary Syndrome (PCOS). While genetic components play a role, exposure to particular environmental stimuli may conceivably impact the activation of genes associated with PCOS, thereby compounding the intricacies of grasping this condition.
Notably, the sphere of concern involves endocrine-disrupting compounds (EDCs), commonly detected in everyday objects like plastics, pesticides and personal care products. These elements possess the capacity to disrupt the hormonal balance, potentially interfering with the endocrine system. It also intensifies the inherent hormonal imbalances linked to PCOS.
Diagnosis and Treatment
Dealing with (PCOS) involves a process that takes into account both the physical and hormonal aspects. Addressing PCOS encompasses a thorough procedure that takes into account both the diagnostic procedure with an exploration of medical history, proper clinical assessment and pertinent tests.
During diagnosis, healthcare practitioners may factor in variables such as irregular menstrual patterns, escalated androgen levels and the presence of ovarian cysts through ultrasound.
Once diagnosed, the management of PCOS aims to address its various symptoms and underlying hormonal imbalances. Lifestyle modifications often form the foundation of treatment, encompassing dietary changes, regular exercise, stress management, sleep regulation and weight management. These measures can help improve insulin sensitivity and regulate hormone levels.
When To Talk To a Specialist
If you suspect that you could be dealing with Polycystic Ovary Syndrome (PCOS) or are encountering symptoms correlated with the condition, seek consultation with a medical expert. While primary care physicians can initiate the diagnostic procedure, there are particular scenarios where seeking advice from a specialist can prove advantageous.
Consider reaching out to a specialist if you experience persistent symptoms like irregular menstrual cycles, excessive hair growth, or acne. Seeking a gynecologist or endocrinologist’s expertise can provide a deeper assessment and personalized guidance tailored to hormonal disorders. If you’re facing difficulties conceiving, consulting a reproductive endocrinologist or fertility specialist is essential, as PCOS can impact fertility and require specialized intervention.
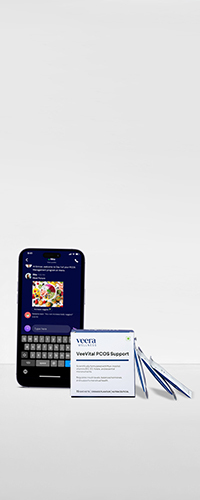
Learn More With Veera
Curious to learn more about PCOS and other related health topics? Look no further than Veera Health — your go-to destination for valuable insights and expert guidance. Swing by our website to dive into a world of information that’s designed to empower you on your health journey.
If you’re facing PCOS issues, searching for effective solutions, or just aiming to improve your overall well-being, we’re here to provide support. Our platform is packed with informative resources, helpful articles and expert guidance. All this is designed to help you understand and manage conditions like Polycystic Ovary Syndrome.
Don’t hesitate. Come visit us at veerahealth.com and take a step toward becoming the healthiest, happiest version of yourself. Let’s start this journey together!