Polycystic ovary syndrome (PCOS) is characterized by an imbalance of reproductive hormones, leading to complications in the ovaries. It is a prevalent condition, affecting around 1 in 10 women of reproductive age in the United States. PCOS can result in irregular menstrual periods, potentially leading to fertility issues. Additionally, individuals with PCOS may sometimes develop cysts in their ovaries.
The immune system is responsive to signals from female reproductive hormones. It appears that levels of hormones, including estrogen and testosterone, and fluctuations in them, can trigger autoimmunity. Autoimmunity is a condition in which the immune system, which typically defends the body against external invaders like infections, instead turns and attacks the body’s tissues such as skin, joints, liver, lungs and more. Autoimmune diseases commonly involve inflammation in various tissues throughout the body.
Understanding Polycystic Ovary Syndrome
Polycystic Ovarian Syndrome, or PCOS, is a prevalent condition that impacts nearly 1 in 5 women. Stemming from a hormonal imbalance, PCOS manifests a spectrum of symptoms affecting menstruation, pregnancy and fertility, skin and hair health, weight and mental well-being. In severe cases, it may lead to complications in cardiovascular health. While the exact cause of PCOS remains uncertain, it is often linked to genetic factors and lifestyle. However, a definitive cure for the condition is not established. The most effective and sustainable approaches to managing PCOS symptoms involve lifestyle adjustments and medical intervention.
An Overview of Joint Pain
Joint discomfort refers to the unease experienced in one or more joints within your body. A joint is the point where two or more bones meet, such as the hip joint where the thigh bone connects with the pelvis.
This discomfort commonly occurs in areas like the hands, feet, hips, knees, or spine. Joint pain can be persistent or intermittent, and individuals may describe sensations of stiffness, achiness, soreness, or even a burning or throbbing feeling. Some may experience a “grating” sensation in their joints. Morning stiffness is also common but often improves with movement and activity. However, excessive activity can exacerbate the pain.
The impact of joint pain goes beyond mere discomfort; it may impede the proper functioning of your joints and restrict your ability to perform everyday tasks. Severe joint pain can significantly affect your quality of life. Therefore, treatment should not only target pain relief but also aim to restore functionality and enable individuals to engage in their daily activities to the fullest extent.
People prone to joint pain often include those with:
- Arthritis or other chronic medical conditions.
- A history of joint injuries.
- Repetitive use or overuse of specific muscles.
- Experiencing depression, anxiety and/or stress.
- Being overweight (with a BMI greater than 25) or obese (with a BMI greater than 30).
- Age plays a role in the development of stiff and painful joints, with issues becoming more common after the age of 45 due to years of joint use and wear and tear.
Exploring the Connection Between PCOS and Joint Health
Hormonal Imbalance
As individuals age, there is a natural decline in estrogen levels, leading to joint swelling that can be notably painful. Menopause, characterized by reduced estrogen levels, has a direct impact on joint health. Estrogen plays a protective role in the joints, maintaining bone integrity and minimizing inflammation. As aging progresses, the diminishing estrogen levels contribute to joint swelling, resulting in considerable discomfort.
Typically, joint pain during menopause is heightened in the morning, when joints are stiff from overnight disuse. Throughout the day, as activity increases, joints tend to become more flexible. The hands, wrists, elbows, jaw and shoulders are particularly prone to being affected. Osteoporosis also plays a role in exacerbating joint issues.
As we age, prioritizing mobility and flexibility becomes increasingly important. If the simple act of getting out of bed becomes challenging, it may be an indication that proactive measures are necessary. Joint pain is a common occurrence with aging, and menopausal women often experience it due to declining estrogen levels. This reduction in estrogen also contributes to decreased bone density. Joint pain is typically accompanied by stiffness, shooting pains, or swelling. When the thyroid functions inadequately, leading to hypothyroidism, specific proteins accumulate in connective tissues, resulting in painful and degenerated joints. This occurrence may be attributed to the release of thyroid-stimulating hormone in response to decreased thyroid gland output. Consequently, thickening and fluid retention affect joints in the hands, feet, ankles and knees, accompanied by bone thinning near the joints.
Conversely, hyperthyroidism (excessive thyroid production) is associated with a rare condition known as acropachy. Symptoms of acropachy encompass finger and toe swelling, clubbing, bulging eyes, rash and bone pain, affecting only a small percentage of individuals with autoimmune thyroid diseases like Graves’ disease. Additionally, hyperthyroidism linked to bursitis, causes a painful condition primarily occurring in the shoulders, restricting joint mobility. A study spanning from 1974 to 2004, involving 33,000 participants aged mid-20s to early 50s, revealed a connection between low testosterone levels and the onset of rheumatoid arthritis.
Moreover, there appears to be an association between rheumatoid arthritis in women and abnormalities in androgen urinary excretion, coupled with low plasma levels of DHEAS (a precursor to testosterone and estrogen). However, further research required to confirm these findings. While evidence suggests a role for testosterone in rheumatoid arthritis, the specific causes remain unknown.
Inflammation
When you experience a joint injury, such as a bruised knee or a sprained ankle, a degree of inflammation is a natural component of the healing mechanism. Swollen, red and tender joints are signs that your immune system is actively eliminating damage and facilitating the growth of new tissue—an essential aspect of healthy inflammation. However, there are instances when the immune system initiates unhealthy, persistent inflammation in the joints without an evident cause. This unwarranted response results in pain, stiffness and joint damage, a condition referred to as inflammatory arthritis.
There are various types of inflammatory arthritis, and some common ones include:
- Rheumatoid arthritis (RA): RA occurs when the immune system targets the lining of joints, particularly in the hands, wrists and feet. It may also impact other organs such as the heart, lungs and eyes.
- Gout: Characterized by an accumulation of uric acid, gout can lead to the formation of crystals in the joints, especially the big toe, and occasionally in the hands, wrists, or knees. These crystals trigger a temporary inflammatory response that may evolve into a chronic condition.
- Calcium pyrophosphate deposition disease (CPPD or pseudogout): In CPPD, calcium crystals settle in the joints, primarily in the knee, wrist, shoulder, ankle, or elbow. Similar to uric acid crystals in gout, these calcium crystals induce inflammation, potentially becoming chronic over time.
- Psoriatic arthritis: Approximately 30% of individuals with psoriasis, an autoimmune condition causing raised patches of scaly skin, develop psoriatic arthritis. This form of arthritis can affect joints like the knees, ankles, wrists, or fingers.
Tips for Managing Joint Pain with PCOS
Meal Planning Holds the Key to a Healthy Diet
Half-sliced vegetables have anti-inflammatory properties, a crucial consideration for managing PCOS, which is significantly influenced by insulin production. Given the link between PCOS and insulin resistance, a condition elevating the risk of diabetes, it becomes essential to integrate meals into your routine that effectively manage insulin levels. Research supports the idea that food choices play a pivotal role in PCOS, urging individuals to carefully plan meals that avoid inflammation triggers and insulin spikes.
Internal nourishment is paramount, prompting a reassessment of your grocery list to include items aligning with a low glycemic index (GI) and an anti-inflammatory diet. The glycaemic index rates carbohydrate-containing foods based on their impact on blood sugar levels. Opt for low-GI foods, such as whole grains, legumes, seeds, nuts and starchy vegetables, to promote a gradual increase in blood sugar levels. Likewise, choose anti-inflammatory foods like tomatoes, olive oil, nuts, leafy greens, fatty fish, healthy oils and fruits to manage PCOS symptoms effectively.
Incorporating Omega-3 supplements into your routine is beneficial for women with PCOS, as they help lower testosterone levels, contribute to inflammation management and possess strong anti-inflammatory effects. Additionally, Omega-3 supplements offer various other advantages, including lowering triglycerides and cholesterol, improving mood, addressing non-alcoholic fatty liver disease, enhancing egg quality and ovulation and reducing androgens.
Engaging in Gentle Exercise for PCOS Joint Pain
Maintaining a healthy weight is crucial for preventing joint pain associated with PCOS. Exercise not only aids in weight management but also provides mental health benefits by reducing stress hormones and releasing endorphins. Aerobic exercises like jogging, walking, cycling, swimming and jump rope are particularly effective.
Utilizing NSAIDs for Inflammation Relief
Nonsteroidal anti-inflammatory drugs (NSAIDs) can effectively alleviate discomfort caused by inflammation by reducing the production of prostaglandins. Taking the recommended dosage before engaging in activities triggering joint pain can preemptively reduce inflammation.
Massage Therapy for Joint Pain Relief
This therapy by a licensed professional can help alleviate joint pain by increasing blood flow and promoting relaxation. Massage therapy may boost serotonin levels and reduce inflammatory cytokines. Consider self-massage with essential oils like lavender oil for a soothing effect on affected areas.
Considering Your Environment for PCOS Management
Optimal work environments are crucial, especially when working from home. Investing in ergonomic furniture and taking regular breaks can prevent exacerbation of joint pain. Avoid prolonged periods of inactivity, and incorporate gentle stretches or short walks into your routine to relieve discomfort.
Alternating Between Heat and Ice for Joint Pain
Alternating between heat and ice applications can provide relief for joint pain. Heat encourages blood flow and nutrient delivery, while cold helps decrease swelling. Ensure the source of heat or cold is wrapped in a flannel to avoid skin irritation. Using a hot water bottle or ice pack for 15–20 minutes on affected areas can be beneficial, but discontinue use if any irritation occurs.
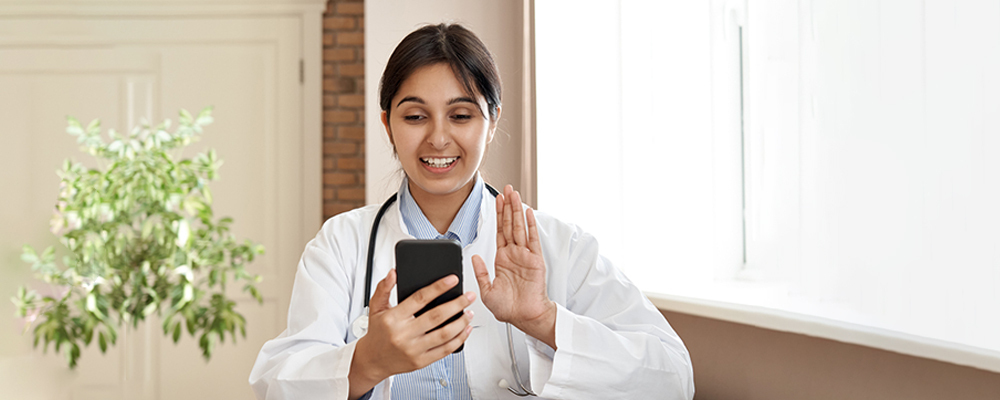
Learn More With Veera
Understanding and implementing treatment choices for PCOS-related symptoms can be challenging due to the absence of a standardized care approach. However, it has been observed that adopting a healthy diet, engaging in regular exercise and incorporating yoga into one’s routine can alleviate symptoms and mitigate the severity of the condition. For specific problems like joint pain, you can consult with Veera Health experts.