The global climate is becoming increasingly unpredictable, posing significant threats to human life through progressive extreme weather events. Human activities and climate change share a reciprocal relationship: our actions contribute to climate change, which in turn impacts global physical activity patterns. Undoubtedly, climate change disrupts the quality of life, affecting health, welfare, food security, and the environment. Unfortunately, the most serious and existential health effects of climate change have been largely underappreciated.
Effects of Climate Change on GI Health
Is there a possible association between climate change and gastrointestinal (GI) health? While the cardiovascular and respiratory systems are often considered primary victims of climate change, GI health is also vulnerable and its impact is underappreciated. Environmental factors could significantly alter GI disease patterns, including inflammatory bowel disease (IBD), functional GI disorders, and GI cancers. Climate change will lead to increased migration, consequently placing a greater burden on the healthcare system. Due to cultural differences, GI healthcare providers will need training in diagnosing and treating unfamiliar diseases. Additionally, overcrowding may pose significant health challenges. Migration also introduces various stress factors that can negatively impact mental health.
Climate change impacts our health in numerous ways, with recent events such as extreme rainfall and floods demonstrating its adverse effects. If unaddressed, these disasters are expected to continue harming our health. A carbon footprint measures the amount of CO2 we generate through our actions. The healthcare sector alone accounts for over 4% of global CO2 emissions, highlighting its significant contribution. The greenhouse effect refers to the natural warming of the Earth caused by atmospheric gases trapping heat from the sun, making the planet habitable. However, excessive atmospheric CO2 and other greenhouse gases from human activities result in additional heat being trapped, causing global warming.
Effects on GI and Liver Physiology
Climate change, particularly extreme heat events, can significantly impact mammalian physiological functions. Individuals with chronic illnesses, such as chronic liver disease, are especially vulnerable to the effects of excessive heat. Reported impacts of extreme heat on the human liver include ischaemia due to peripheral vasodilatation aimed at dissipating heat. This can lead to hepatocyte necrosis resulting from ischaemia and hypoxia caused by compensatory splanchnic vasoconstriction, as well as direct cytotoxicity, potentially causing acute liver injury and, in severe cases, acute liver failure. Extreme heat-induced cytotoxicity has also been linked to pancreatitis and damage to the intestinal mucosal barrier, increasing permeability and leading to endotoxaemia. Furthermore, climate change affects epithelial barriers across all mucosal surfaces through thermal toxicity to epithelial cells and altered splanchnic circulation, causing oxidative stress. This can result in diarrhoea, dehydration, dyselectrolytaemia, and, ultimately, death.
Climate Change and Functional GI Disorders
Climate change closely affects mental health, with acute stress from events like wildfires, floods, and storms compounded by chronic stress from struggles to secure food, water, and shelter. Mental health is strongly linked to functional GI disorders, which are among the most common GI issues in the population. Acute dysbiosis can cause mild abdominal pain and diarrhoea, while chronic dysbiosis can increase the risk of inflammatory bowel disease (IBD), celiac disease, and other autoimmune disorders. Changes in gut microbiota are closely related to disease patterns, and understanding how climate change affects gut microbiota is crucial. Increased CO2 production alters soil composition, affecting food nutrients and ultimately changing our gut microbiota, which plays a significant role in the patterns of GI disorders.
Climate Change and Diarrhea
Rising temperatures and flooding can lead to an increase in waterborne diseases such as cholera, affecting both low-income and high-income countries. Heavy rains can disrupt drainage systems, contaminate drinking water, and increase intestinal infections. Diarrheal diseases are a leading cause of death in children, and the World Health Organization (WHO) estimates that by 2050, approximately 33,000 children under the age of 15 could die from diarrheal diseases due to climate change. Water pollution caused by climate change can expose people to pathogens responsible for waterborne and vector-borne infections. Elevated temperatures can also lead to outbreaks of salmonella and campylobacter, while harmful algae such as cyanobacteria can cause GI problems.
Can We Have a Positive Gut Reaction to Nature?
Pioneering studies, such as those conducted with mice, demonstrate that the influence of the microbiome extends far beyond the gut, reaching the mind. This research adds to decades of studies on the gut-brain axis, the biochemical signalling pathway between the gastrointestinal tract and the central nervous system, which influences our moods, behaviours, cravings, and repulsions.
Breed suggests that our microbiome may have an even broader impact. Studies indicate that people who spend more time in nature during childhood are more likely to develop biophilic traits as adults. The “lovebug hypothesis” proposes that this positive feedback loop might be driven by symbiotic gut microbes acquired from the outdoor environment. Interacting with nature may benefit both humans and gut microorganisms. These microbes rely on us to complete their life cycle, and Breed speculates humorously that they might be “manipulating” us to enjoy returning to nature. People who grow up with better access to nature tend to engage in behaviours that would support the life cycles of these microbes.
If such interactions between the micro and macro environments are common, urban microbiome rewilding projects, especially in socioeconomically deprived areas, could foster a love of nature in a new generation of city children. These projects could also help address socioeconomic disparities in health and well-being. Microbiome research is a bold new frontier, reinforcing the adage “We are what we eat,” while also suggesting new truths: “We are what we breathe,” “We are what we experience,” and possibly much more.
Diet and Gut Microbiota
The gut microbiota comprises a complex community of beneficial and pathogenic microorganisms. Diet significantly influences the composition and diversity of these microorganisms. Macronutrients such as fats, proteins, carbohydrates, and fibre distinctly impact gut microbiota.
The role of probiotics and prebiotics in gut health has been extensively researched. Probiotics are live microorganisms that confer health benefits by maintaining gut microbiota balance when consumed in adequate amounts. Prebiotics are non-digestible food components that promote the growth and activity of beneficial gut bacteria. The interaction between probiotics and prebiotics is essential for producing short-chain fatty acids, which support intestinal barrier integrity, gut hormone secretion, inflammation prevention, cancer risk reduction, and chromatin regulation.
Research shows that probiotics can influence cellular aging and degeneration through their nutritional and immunomodulatory properties, indicating that diet can impact the aging process via the gut microbiota. Poor nutritional status leading to gut microbiota changes can significantly affect overall health.
Gut Microbiota and Human Aging
The gut microbiota plays a crucial role in regulating metabolism, the immune system, and the neuropsychiatric system. An imbalance in gut microbiota composition (dysbiosis) can lead to health issues. Recent models highlight a link between gut microbiota dysbiosis and ageing. Reduced levels of butyrate-producing microbes are associated with various health conditions. Although microbiota diversity increases with age, older adults often have fewer core bacterial species.
Reduced short-chain fatty acid and secondary bile acid production, along with increased lipopolysaccharide production, can cause chronic low-grade inflammation, a hallmark of many age-related diseases. The gut-brain axis involves communication pathways like the vagus nerve, enteric nervous system, immune system, and tryptophan metabolism, with metabolites such as short-chain fatty acids, branched-chain amino acids, and peptidoglycans playing key roles.
An imbalance in gut bacteria can affect physical health in ageing by inducing inflammation, reducing muscle mass, altering lipid metabolism, and lowering vitamin levels. Beneficial bacterial communities are linked to anti-inflammatory responses, better mitochondrial function, and increased short-chain fatty acid production.
Gut microbiota dysbiosis can also impact cognitive functions and psychological well-being, potentially increasing cerebrospinal fluid biomarkers, lipopolysaccharide levels, and amyloid deposition in the brain, which are associated with neurodegenerative diseases like Alzheimer’s. Additionally, dysbiosis can disrupt metabolic processes, leading to fat accumulation, insulin resistance, and glucose intolerance, which are linked to obesity, diabetes, and other metabolic disorders. Numerous studies have validated the bidirectional relationships between climate change and gut microbiota, as well as between gut microbiota and ageing. However, few studies have examined the direct correlation between climate change and ageing.
This highlights the need for more comprehensive evidence regarding the relationship between climate change and ageing, despite the strong linkage through gut microbiota. Future research should investigate the impact of various climate change components, such as air quality and humidity, in addition to temperature, on gut microbiota and ageing in biologically relevant animal models.
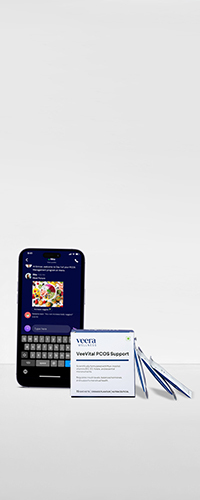
Learn More With Veera
Prioritizing a healthy gastrointestinal lifestyle is essential for overall well-being and disease prevention. Emphasize fibre, stay hydrated, incorporate prebiotics and probiotics, exercise regularly, manage stress, practice good hygiene, get enough sleep, and avoid smoking, alcohol, and processed foods. Adhering to these guidelines boosts physical, mental, and emotional health, with support from Veera Health’s expert gynaecologists.