If you have a uterus, you are likely acquainted with cramps. But if you are wondering why you get them in the first place. It happens because the uterus lining builds up throughout the cycle, then sheds during your periods if an egg is not fertilised. The uterus responds with cramping as a way to control the bleeding. That said, period pains are pretty subjective as different women have different tolerance to pain but may also be due to conditions such as endometriosis or fibroids. If you cannot get out of your bed and go to work, here are all the reasons why your periods may hurt so badly.
If You Have Heavy Flow with Agonising Cramps
What it could be: If you get heavy flow with awful cramps, it might be uterine fibroids. Fibroids are benign growths that grow in and around the wall of the uterus. They increase and distort the surface of the uterine lining, which can make the bleeding and cramping super-intense during your periods. Sometimes if you have a very heavy flow during your period, it can make you anaemic, making you feel more tired than normal.
What to do: Fibroids can be genetic, so, see your doctor if there has been a history of these benign growths in your family. Your ob-gyn will likely send you for an ultrasound to check for the size and locations of them. To minimise the pain and heavy flow during your periods, most doctors prescribe birth control pills with over the counter medications such as ibuprofen. For particularly severe cases, you might need to undergo surgery depending on the size and the location of the fibroids. To prevent anaemia, your doctor may advise you to take iron supplements and will regularly check your haemoglobin and blood counts.
If You Have Cramps That Medications Don’t Help
What it could be: If over-the-counter medications don’t give you any relief, you should consider endometriosis. The condition causes the uterine lining, called the endometrium, to grow on other organs such as the uterus, fallopian tubes, ovaries, even your abdominal wall and intestines.
What to do: If you can, keep a log of the degree of pain as well as the date of your periods. The more information you can provide about your cycle, the easier will it be for the doctor to diagnose the problem. But if you are very uncomfortable, see a doctor immediately. Your ob-gyn will prescribe hormone treatments to decrease the duration of your period and reduce the amount of pain you experience each month.
If You Have Dull, Constant Pain
What it could be: A constant pain outside of your menstrual cycle accompanied by a vaginal discharge could be a sign of PID or pelvic inflammatory disorder. PID is an infection of the uterus, ovaries, or fallopian tubes that is often a result of untreated STDs like chlamydia or gonorrhoea.
What to do: Your doctor will recommend a swab culture to check for bacteria or an infection. Doctors cure PID with antibiotics, but when you leave it untreated, it can form scar tissue in your reproductive tract and interfere with your fertility or cause an ectopic pregnancy (a pregnancy that develops outside of the uterus).
If You Have Sharp Pain on One Side
What it could be: Sudden, sharp pain or stabbing pain on one side could be a sign of a ruptured ovarian cyst or an ovarian torsion. Ovarian cysts are pretty harmless unless they rupture or break open. Ovarian torsion is also a serious condition where an ovarian cyst causes the ovary to twist, cutting off the blood flow to the ovary. Sometimes, nausea and vomiting too can accompany the pain. This type of pain doesn’t necessarily have to accompany your periods.
What to do: Go straight to the emergency room and get the necessary scans done to determine the cause of the pain. While the treatment for ruptured cysts can vary from mild interventions to surgery, you will pretty much need to go under the knife if it’s an ovarian torsion.
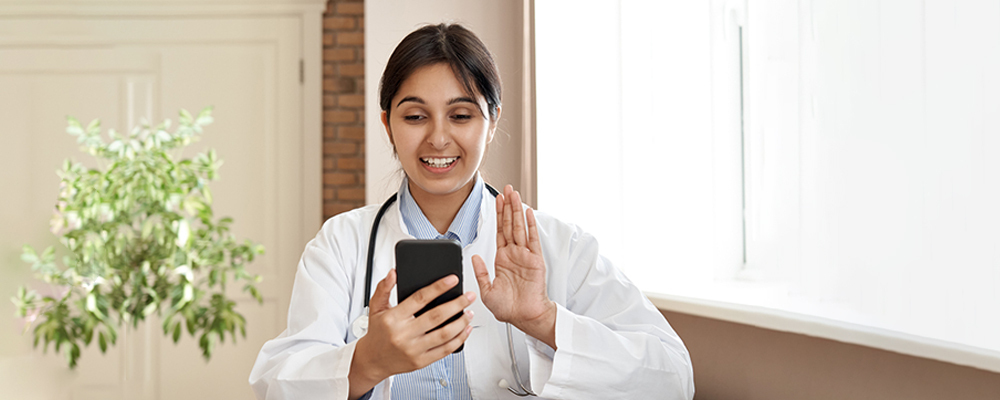
Also, any cramping or bleeding outside your normal cycle could be a cause for suspicion. It could be a warning sign for ectopic pregnancy or a miscarriage. Read more about miscarriages and ectopic pregnancy on our website. If you have painful periods, talking with our Veera gynaecologists can help you figure out the cause and how to manage it.
References:
[1] Bernardi, M., Lazzeri, L., Perelli, F., Reis, F. M., & Petraglia, F. (2017). Dysmenorrhea and related disorders. F1000Research, 6, 1645. https://doi.org/10.12688/f1000research.11682.1[2] Proctor, M., & Farquhar, C. (2006). Diagnosis and management of dysmenorrhoea. BMJ (Clinical research ed.), 332(7550), 1134–1138. https://doi.org/10.1136/bmj.332.7550.1134[3] Rosenwaks Z, Seegar-Jones G. Menstrual pain: its origin and pathogenesis. JReprod Med. 1980 Oct;25(4 Suppl):207-12. Review. PubMed PMID: 7001019.[4] Sharghi, M., Mansurkhani, S. M., Larky, D. A., Kooti, W., Niksefat, M., Firoozbakht, M., Behzadifar, M., Azami, M., Servatyari, K., & Jouybari, L. (2019). An update and systematic review on the treatment of primary dysmenorrhea. JBRA assisted reproduction, 23(1), 51–57. https://doi.org/10.5935/1518-0557.20180083
Disclaimer: Content on Veera is provided for informational purposes only and is not intended as medical advice, or as a substitute for medical advice given by a physician